
Choosing the right occupational therapy assessment sets the stage for evidence-based OT practice.
But, finding the right combination of assessments can take a little digging, as there are more OT assessment tools out there than you may realize. Many are disease- or condition-specific, and many approach the assessment process from different angles (top-down, bottom-up, questionnaire style, etc.). Therapists should also consider if a self-report measure might be a helpful way to establish your client as a partner in care.
Luckily, many of these assessments are FREE. 🙂
We are so passionate about helping OTs find the right assessment to kick-start their care. In this post, you’ll learn about our OT Assessment Search, and get to see a long list of the assessments found in it!
Occupational Therapy Assessment Search in the OT Potential Club
At OT Potential, we want to make it easy for you to deliver the best care possible. And, so we’ve gathered a list of standardized assessments that we found in influential OT-related research studies.
You will find these assessments listed below. Some of them will be familiar, but I suspect you’ll also discover some new ones you’ll be eager to integrate into your practice.
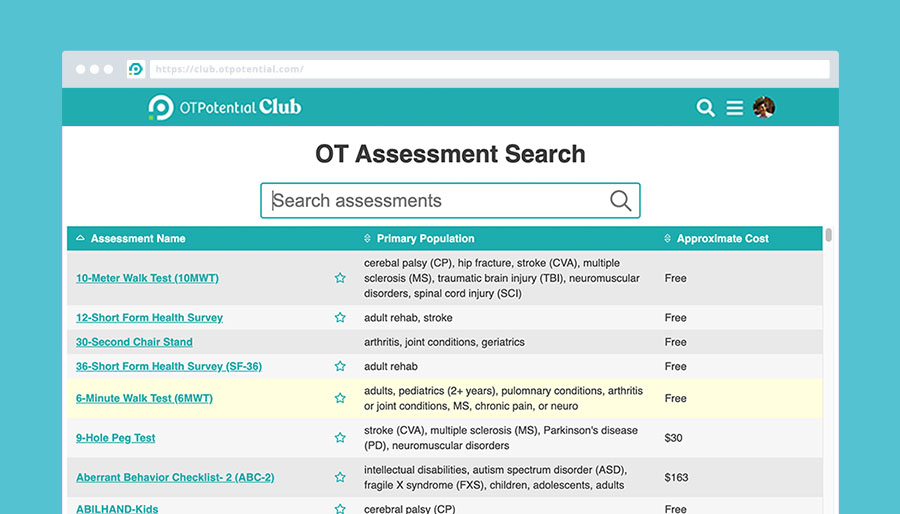
For members of the OT Potential Club, we took things one step further, compiling everything into a comprehensive OT Assessment Search. You’ll be able to quickly find the perfect assessment to kick off your treatments.
For each assessment, you’ll be able to quickly see:
- Primary patient population
- What it assesses
- How much it costs
- How long it takes to administer
- If you need special training beyond your OT degree
Try our OT Assessment Search Tool FREE for 5 days!
Quickly search over 260 OT assessments.
Our ultimate list of occupational therapy assessments!
These assessments were either found in the in the research we’ve reviewed in the OT Potential Club, or were suggested by Club members!
- 6-Minute Walk Test (6MWT)
- 9-Hole Peg Test (9HPT)
- 10-Meter Walk Test (10MWT)
- 12-Short Form Health Survey
- 30-Second Chair Stand Test
- 36-Short Form Health Survey (SF-36)
- Aberrant Behavior Checklist | Second Edition (ABC-2)
- ABILHAND-Kids
- Action Research Arm Test (ARAT)
- Activity Card Sort (ACS)
- Activity Measure for Post-Acute Care
- Addenbrooke’s Cognitive Examination (ACE-III or ACE-R) – (The Short Form)
- Adolescent/Adult Sensory Profile
- Ages and Stages Questionnaire
- AIR Self-Determination Assessment
- Agitated Behaviors Scale-Modified
- Alberta Infant Motor Scale (AIMS)
- American Spinal Cord Injury Association (ASIA) Impairment Scale
- ARC Self-Determination Scale
- Armstrong Neurodiversity Strengths Checklist
- Assessment, Evaluation, and Programming System for Infants and Children
- Assessment of Communication and Interaction Skill (ACIS)
- Assessment of Learning Powered Mobility
- Assessment of Life Habits (Life-H)
- Assessment of Motor and Process skills (AMPS)
- Assisting Hand Assessment (AHA)
- Australian Pelvic Floor Questionnaire
- Autism Diagnostic Observation Schedule™ (ADOS)
- Barthel Index for Activities of Daily Living
- Batten Observational Pain Scale (BOPS)
- Bayley Scales of Infant and Toddler Development
- Beck Depression Inventory (BDI)
- Beery-Buktenica Developmental Test of Visual-Motor Integration | Sixth Edition (BEERY™ VMI)
- Behavioral and Emotional Rating Scale
- Behavior Problems Inventory
- Behavior Rating Inventory of Executive Function (BRIEF)
- Berg Balance Scale (BBS)
- Body Mass Index (BMI)
- Borg Dyspnea Scale
- Boston Carpal Tunnel Outcomes Questionnaire (BCTQ)
- Box and Block test (BBT)
- Brief Autism Mealtime Behavior Inventory (BAMBI)
- Brief Confusion Assessment Method (bCAM)
- Brief Pain Inventory (BPI)
- Bruininks-Oseretsky Test of Motor Proficiency | Second Edition (BOT™-2)
- Canadian Occupational Performance Measure (COPM)
- Caregiver Strain Scale (CSI)
- Casey Life Skills
- Cerebral Palsy Quality of Life Questionnaire (CPQOL)
- Center for Epidemiologic Studies Depression Scale (CES-D)
- Child Occupational Self Assessment (COSA)
- Children’s Assessment of Participation and Enjoyment (CAPE) and Preferences for Activities of Children (PAC)
- Children’s Eating Behavior Inventory
- Children’s Hand‐use Experience Questionnaire (CHEQ)
- Children’s Sleep Habits Questionnaire (CSHQ)
- Children Hospital of Philadelphia Infant Test of Neuromuscular Disorders (CHOP INTEND)
- Children’s Depression Inventory, Second Edition (CDI 2)
- The Chronic Pain Acceptance Questionnaire (CPAQ-8)
- Clinical Assessment of Modes
- Clinical Disease Activity Index (CDAI)
- Clinical Global Impressions – Improvement Scale (CGI-I)
- Cognitive Failures Questionnaire (CFQ)
- Confusion Assessment Method for the ICU (CAM-ICU)
- Connection to Nature Index (CNI)
- Consultation and Relational Empathy (CARE) Measure
- Dallas Pain Questionnaire
- Dartmouth COOP Charts
- DeCoste Writing Protocol (DWP)
- Dementia Screening Questionnaire for Individuals with Intellectual Disabilities
- Depression, Anxiety, and Stress Scale
- Developmental Assessment of Young Children | Second Edition (DAYC-2)
- Developmental Behavior Checklist for Adults
- Developmental Coordination Disorder – Questionnaire (DCDQ)
- The Developmental Profile (DP-4)
- Developmental Test of Visual Perception (DTVP-3)
- Devereux Behavior Rating Scale (DBRS™)
- Disabilities of the Arm, Shoulder and Hand (DASH)
- Distress Thermometer
- Dynamic Assessment of Social Emotional Learning (DASEL)
- Early Learning Accomplishment Profile – E-LAP
- Edinburgh Postnatal Depression Scale (EPDS)
- Edmonton Symptom Assessment Scale (ESAS)
- European Quality of Life – 5 Dimensions (EQ-5D)
- Evaluation Tool of Children’s Handwriting (ETCH)
- Everyday Technology Use Questionnaire
- Expanded Disability Status Scale (EDSS)
- Falls Efficacy Scale – International (FES-I)
- Family Resource Scale
- Family Support Scale
- Female Sexual Function Index (FSFI)
- Four Square Step Test (FSST)
- Frenchay Activities Index (FAI)
- Fugl-Meyer Assessment of Motor Recovery After Stroke (FMA)
- Functional Assessment and Curriculum for Teaching Everyday Routines (FACTER)
- Functional Assessment of Cancer Therapy – Breast (FACT-B)
- Functional Assessment of Cancer Therapy – Cognitive Function (FACT-Cog)
- Functional Assessment of Cancer Therapy: General (FACT-G)
- Functional Assessment of Chronic Illness Therapy – Fatigue (FACIT-F)
- Functional Emotional Assessment Scale (FEAS)
- Functional Independence Measure (FIM)
- Functional Simulated Technology Task
- General Health Questionnaire (GHQ)
- General Self-Efficacy Scale (GSE)
- Geriatric Depression Scale (GDS)
- Goal Attainment Scaling (GAS)
- Goal Oriented Assessment of Life Skills (GOAL)
- Grip Strength
- Gross Motor Function Measure
- Guy’s Neurological Disability Scale (GNDS)
- Hamilton Rating Scale for Depression (HAM-D)
- Hammersmith Functional Motor Scale Expanded (HFMSE)
- Hammersmith Neonatal Neurological Examination (HNNE)
- Hawaii Early Learning Profile (HELP)
- Health Assessment Questionnaire- Disability Index
- Heart Drawing Tool
- Hospital Anxiety and Depression Scale (HADS)
- Independent Living Scales™ (ILS™)
- Infant-Toddler Social and Emotional Assessment (ITSEA)
- Jebsen-Taylor Test of Hand Function (JTTHF)
- Jordan Left-Right Reversal Test
- Karnofsky Performance Scale
- Katz Index of Independence in Activities of Daily Living (Katz ADL)
- Kohlman Evaluation of Living Skills
- Lawton Instrumental ADL Scale (IADL)
- Little Developmental Coordination Disorder Questionnaire
- London Handicap Scale (LHS)
- MacArthur-Bates Communicative Development Inventories (MB-CDIs)
- Manual Ability Measure (MAM-36)
- Maternal Self-Efficacy Scale (MSES)
- McMaster Family Assessment Device
- McMaster Handwriting Assessment Protocol (MHAP)
- Mealtime Behavior Questionnaire (MBQ)
- Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36)
- The Medi-Cog
- Melbourne Assessment of Unilateral Upper Limb Function (MUUL)
- Mental Health Screening Form III
- Miller Behavioral Style Scale (MBSS)
- Miller Function and Participation Scales (M-FUN)
- Mini-Cog©
- Mini-Mental State Exam (MMSE)
- Modified Ashworth Scale (MAS)
- Modified Checklist for Autism in Toddlers (M-CHAT)
- Modified Rankin Scale (mRS)
- Montgomery-Asberg Depression Rating Scale (MADRS)
- Montreal Cognitive Assessment (MoCA)
- Motion Sensitivity Quotient/Test (MSQ/MST)
- Motor Activity Log (MAL)
- Motor Function Measure (MFM)
- Motricity Index for Motor Impairment After Stroke
- Movement Assessment Battery for Children | Second Edition Movement ABC-2
- MS Quality of Life 54 (MSQOL 54)
- Mullen Scales of Early Learning (MESL)
- Multidimensional Anxiety Scale for Children | Second Edition (MASC 2)
- National Institutes of Health Stroke Scale (NIHSS)
- Neurobehavioral Functioning Inventory (NFI)
- Non-Communicating Adult Pain Checklist
- Non-Communicating Children’s Pain Checklist (NCCPC)
- Nottingham Extended Activities of Daily Living (NEADL) Scale
- Nottingham Health Profile (NHP)
- Nottingham Leisure Questionnaire (NLQ)
- The Occupational Experience Profile (OEP)
- Occupational Performance History Interview-II (OPHI-II)
- The Occupational Self Assessment (OSA)
- Pain Assessment in Advanced Dementia Scale (PAINAD)
- Pain Catastrophizing Scale (PCS) (child version and parent version)
- Pain Disability Index
- Pain Self-Efficacy Questionnaire (PSEQ)
- Parenting Sense of Competence Scale (PSOC)
- Parenting Stress Index – Short Form (PSI-SF)
- Parkinson’s Disease Questionnaire – 39 (PDQ-39)
- Participation Assessment and Recombined Tools (PART-O)
- Patient Health Questionnaire (PHQ-9)
- Patient-Rated Wrist Evaluation (PRWE)
- Patient-Specific Functional Scale (PSFS)
- Peabody Developmental Motor Scales (PDMS)
- Pediatric Activity Card Sort (PACS)
- Pediatric Confusion Assessment Method for the Intensive Care Unit (pCAM-ICU)
- Pediatric Evaluation of Disability Inventory (PEDI)
- Pediatric Interest Profiles (PIP)
- Pediatric Pain Profile (PPP)
- The Pediatric Quality of Life Inventory (PedsQL)
- Pediatric Quality of Life Questionnaire (PedsQL)
- Pelvic Floor Disability Index (PFDI-20)
- Pelvic Floor Impact Questionnaire (PFIQ-7)
- Perceived Change Index (PCI)
- Perceived Efficacy and Goal Setting System (PEGS)
- Perceive, Recall, Plan, and Perform System (PRPP)
- Personal Adjustment and Role Skills (PARS)
- The Personal Recovery Outcome Measure (PROM)
- Pervasive Developmental Disorders Behavior Inventory (PDDBI)
- Photovoice process
- Physical Function in the ICU – Scored (PFIT-s)
- Pinch Strength
- Piper Fatigue Scale (PFS)
- Pittsburgh Agitation Scale (PAS)
- Positive and Negative Affect Scale (PANAS)
- Postpartum Social Support Screening
- Postural Assessment Scale for Stroke Patients (PASS)
- Preschool Confusion Assessment Method for the ICU (psCAM-ICU)
- Preschool Language Scales | Fourth Edition (PLS™-4)
- PROMIS Anxiety
- PROMIS Depression
- PROMIS Physical Function Mobility short form
- Quality of Life of in Alzheimers Disease (QoL-AD)
- Quality of Upper Extremity Skills Test (QUEST)
- QuickDASH
- Quick Neurological Screening Test (QNST)
- Rapid Assessment Test for Delirium (4AT)
- Rating of Anxiety in Dementia (RAID)
- REEL-4: Receptive-Expressive Emergent Language Test
- Reintegration to Normal Living Index
- Revised Upper Limb Module (RULM)
- Richmond Agitation-Sedation Scale (RASS)
- Rivermead Mobility Index (RMI)
- Roland Morris Disability Questionnaire
- Roll Evaluation of Activities of Life (REAL™)
- Rosenburg Self-esteem Scale
- Routine Assessment of Patient Index Data 3 (RAPID3)
- Rowland Universal Dementia Assessment Scale 11 (RUDAS)
- Saint Louis University Mental Status Examination (SLUMS)
- Satisfaction with Life Scale (SLS)
- SCA Functional Index (SCAFI)
- Scale for the Assessment and Rating of Ataxia (SARA)
- Scale for the Assessment of Negative Symptoms (SANS)
- Schoodles: Fine Motor & Keyboarding
- School Function Assessment (SFA)
- SCI Falls Concern Scale (SCI-FCS)
- Screen for Child Anxiety Related Disorders (SCARED)
- Self-Directed Search
- Self-Efficacy for Managing Chronic Disease
- Self Perception Profile for Children (SPPC)
- Sensory Integration and Praxis Tests (SIPT)
- Sensory Integration Inventory–Revised for Individuals with Developmental Disabilities
- Sensory Processing Measure (SPM™)
- Sensory Profile™ 2
- Sharpened Romberg (SR)
- Short Blessed Test (SBT)
- The Short Child Occupational Profile (SCOPE)
- Sickness Impact Profile (SIP)
- Social Communication Questionnaire (SCQ)
- Social Responsiveness Scale™ | Second Edition (SRS™-2)
- Spence Children’s Anxiety Scale (SCAS)
- Spinal Cord Independence Measure (SCIM)
- Standardized Touchscreen Assessment of Cognition (STAC)
- Stanford Chronic Disease Self-Efficacy 6-Item Scale (SSE) (SEMCD)
- Stroke Impact Scale (SIS)
- Supports Intensity Scale
- Symbol Digit Modalities Test (SDMT)
- Tampa Scale of Kinesiophobia (TSK)
- Test for Information Processing Skills
- Test of Gross Motor Development (TGMD)
- Test of Infant Motor Performance
- Test of Visual Perceptual Skills (non-motor) | Fourth Edition (TVPS-4)
- Timed Up and Go (TUG) Test
- UCLA PTSD Reaction Index
- Unified Multiple System Atrophy Rating Scale (UMSARS)
- Unified Parkinson’s Disease Rating Scale (UPDRS)
- Vineland Adaptive Behavior Scales | Third Edition (Vineland-3)
- Visual Activity Sort
- Volitional Questionnaire
- WeeFIM
- WHO Quality of Life (WHOQOL)
- Wide Range Assessment of Visual Motor Abilities (WRAVMA)
- Wolf Motor Function Test (WMFT)
- Worker Role Interview
- World Health Organization Disability Assessment Schedule 2.0 (WHODAS 2.0)
- Work and Social Adjustment Scale (WSAS)
- Young Children’s Participation and Environment Measure (YC-PEM)
- Your Current Life Situation Survey
Pediatric assessments and other common practice area-specific options
In our guides to specific OT practice areas, we list common assessments in each setting. These guides are another great starting point for your search to find the right assessment.
- What is acute care occupational therapy?
- Occupational Therapy in Schools (Guide + Directory)
- Occupational Therapy for Adults
Assessments for OTs using telehealth
In light of COVID-19 and the shift toward offering virtual services, we have also gathered information on OT assessments for telehealth care delivery.
Conclusion
Choosing the right assessment sets you up to provide great care—but finding the right one for your needs can be a challenge. At OT Potential, we seek to collect the scattered and hard-to-decipher information on various assessments and make it simple for you to find what you need in just a few clicks.
Please comment below with features you would like to see in The OT Potential Club Assessment Search, as well as your favorite assessments you think we should add to our list.
To get instant access to this growing database of OT-specific assessments, join the OT Potential Club!
Or try the OT Assessment Search Tool today!

11 replies on “Occupational Therapy Assessments (2024)”
Lacls and Ocairs please
Oh yeah! I’ve used both of these! I will add them to my list! Thank you so much!!
De Paul Questionnaire for ME/CFS and Log Covid https://csh.depaul.edu/about/centers-and-institutes/ccr/myalgic-encephalomyelitis-cfs/Documents/DEPAUL%20SYMPTOM%20QUESTIONNAIRE%20with%20SF-36%20and%20MFI%20and%20SI%205-18-11.pdf
QEESI – https://tiltresearch.org/qeesi-2/
NASA lean test for orthostatic intolerance: https://batemanhornecenter.org/assess-orthostatic-intolerance/#:~:text=Ask%20the%20patient%20to%20remove,vital%20readings%20are%20relatively%20consistent.
2 day CPET test for fatigue disabilities eg long covid, ME/CFS, MS etc https://workwellfoundation.org/wp-content/uploads/2023/01/CPET-Methodology-for-Assessing-Exertion-Intolerance-in-MECFS-2018.pdf
Would love to see cited reliably/validity measures, as available for each assessment.
Additionally, it would be great to be able to plug in some key words (such as "dementia", "home safety") in order to quickly identify assessments relating to the search criteria.
Looking forward to seeing where this goes!
Love this feedback, Kori! Thank you!
The search component you mentioned is definitely possible and something we are building.
My plan right now reliability/validity measures is to provide links to pages that contain that information, but not to host it within the search itself…. I’m trying to balance keeping the information easy to read, but having avenues to dive really deep into the assessment.
Oh! And, one more thought on this! I do plan to provide an easy visual, like a star, if the assessment is used in the influential research we review each week in the OT Potential Club. I figure this should serve as an initial indicator of validity/reliability, as one would hope that researchers are only choosing assessments with established validity/reliability.
Hello, I read that you were building a new search component for the assessments, a key word search specifically. Has this been implemented yet?? Thank you
Hi Laura!! Yes! The search is live and we are adding to it every week! The upcoming feature I’m most excited about is that we are categorizing the assessment as top-down vs. bottom-up. Are you a member of the OT Potential Club? The Search has been such a big project, we decided to offer it to our members within the Club. You can learn more here about signing up: https://otpotential.com/
What a great resource! Have you considered including the Occupational Performance Inventory of Sexuality and Intimacy (OPISI)? It can be downloaded for free from opisi.uindy.edu
TVPS -4 is now outdated. Do you have access/info on the most up to date version #5?
Thank you, Mary!! We are planning a big update to this post in July and will be sure to make sure the TVPS gets updated!