We can all probably agree that the most important element in providing quality occupational therapy is a thorough evaluation. And, as with in-person evals, one of the first considerations for any telehealth OT eval should be which assessment(s) you use.
This post will walk you through considerations for choosing the right telehealth assessments—and it will provide some examples of ones that have proven effective in the online setting.
Disclaimer/update on the ever-evolving nature of telehealth OT
Considering the relatively recent emergence (and popularity) of telehealth rehabilitation, much is yet to be learned regarding the effectiveness of providing OT online. The available information is also quickly evolving, so please verify all information before incorporating it into your treatments.
How to choose, how to choose… (6 areas to consider as you choose an assessment)
There are so many OT assessments out there, it can feel absolutely overwhelming. Luckily, certain factors can help us quickly determine whether specific assessments will work for telehealth setups.
We should approach this process by considering whether an assessment is feasible.
An assessment’s feasibility really depends on whether it can be administered remotely. Here are some factors to consider regarding remote assessments:
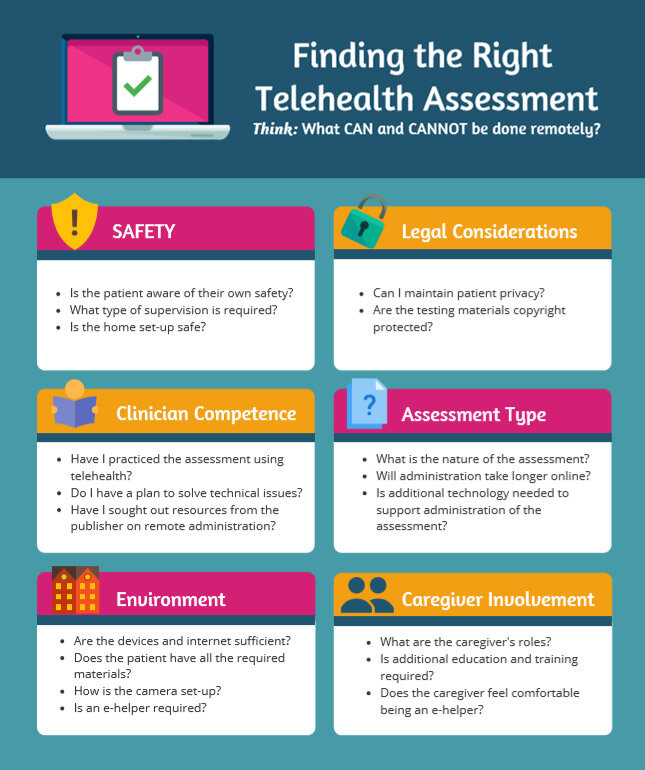
1.) Is it SAFE?
Patient safety is always the first thing you should consider when selecting an assessment, regardless of the mode of delivery. When you administer assessments remotely, things get more complicated: patients and caregivers are now responsible for the environmental setup and supervision (with therapist direction and oversight). This shift in responsibilities requires more instruction and preparation time in order to ensure patient safety.
Consider these telehealth-related safety questions:
- Does the patient have awareness of their own safety?
- How much supervision is required for the patient to be safe?
- Think about the type of supervision needed (e.g. standby assist vs. contact guard), as well as who will be providing that supervision.
- Is the environment safe?
- How much space is required to complete the assessment?
- Is the space free of hazards, clutter, etc.?
2.) What are the LEGAL considerations?
You’ve probably wondered whether you can really maintain a patient’s privacy when delivering telehealth OT. That’s a valid concern.
In response to COVID-19, the US Department of Health and Human services has announced flexibility around HIPAA requirements when shifting to a telehealth service model, meaning that they won’t enforce penalties for violations in accordance with the Health Insurance Portability and Accountability Act of 1996.
There has been no official announcement regarding the expiration of these flexibilities, but things could change at any time. With that in mind, it is definitely advisable that you start thinking about how to protect your patients’ privacy when using telehealth.
Consider these questions:
- Do I have sufficient knowledge of best practices for telehealth?
- Am I using a HIPAA-compliant platform?
- Are the methods in which I am exchanging testing materials and storing completed testing materials secure (e.g. password-protected, encrypted)?
- Are the testing materials I’m using copyright protected?
Some testing materials are protected by copyright laws that prohibit the reproduction of tests, either on paper or electronically, without prior approval. Definitely look at copyright laws for any assessments you consider, and reflect on whether you have the right to use the test(s) you’ve selected.
Provided below is a list of popular publishing companies, where you can find more information regarding legal policies and copyright-protected materials:
3.) Do you feel COMPETENT implementing the assessment via telehealth?
Competency is different from safety. Being competent means that you can perform the test correctly to yield expected results. This means everything from having the right credentials to administer the test to ensuring that you have a solid tech setup. Some of the publishing companies discussed previously have telehealth resources and support for remote administration. (See Pearson’s “Telepractice Overview” and WPS’ “Telepractice Overview.”)
Here are some best-practice questions to consider prior to administering an assessment via telehealth:
- Do I have the current licensure/credentials/training required to administer the test?
- How will I provide clear and concise instructions via telehealth?
- Do I have a contingency plan in place to resolve technical issues?
- Have I reviewed the publisher’s website for specific tips and/or requirements for remote administration? (This is especially important if you are unclear on how an assessment can be implemented through a telehealth platform.)
4.) What is the NATURE of the assessment?
It’s OK to admit that some OT assessments might not work for telehealth. That’s why many telehealth practitioners will opt for a simple questionnaire vs. an assessment that requires a lot of testing materials. In fact, we’d argue that choosing tests that are more observational in nature might be the best starting point.
Here is a list of questions to consider when deciding on a telehealth OT assessment:
- Is the test valid and reliable for use through telehealth?
- Does the assessment consist of tabletop work and questionnaires? Or does it require physical demonstrations and gross motor tasks?
- What are the required testing materials?
- Is the assessment paper-based? Or are additional items and materials required?
- Are the materials easily available within the home?
- How will I send and retrieve the standardized testing materials and forms?
- How much time does the assessment take to complete?
- You may want to anticipate the assessment taking longer when you use a telehealth platform.
- Is additional technology needed to support the administration of the assessment?
5.) Is the home ENVIRONMENT conducive to the assessment?
The home environment needs to be set up in a way that best supports both the patient and the clinician, especially when it comes to the administration of the assessment(s) you use.
Consider these questions in preparation for administering an assessment through telehealth:
- What type of device/internet connection is the patient using?
- Consider potential barriers with positioning, screen size, camera quality, and internet speed. (Patients with <1 MBps connection speed may experience lagging.)
- Does the patient have all the required testing materials?
- Consider how you will send and retrieve those items, as well as any disinfecting protocols.
- Do I require assistance from an e-helper?
- An e-helper can be a parent or caregiver whose physical presence can support the success and smoothness of the telehealth session. E-helpers may require additional training in the testing procedures and technologies you are using.
- If you require an e-helper, consider what training and testing instructions (written/verbal) you will need to provide them prior to your testing session.
- How will I address the need for a distraction-free environment?
6.) If you need CAREGIVER involvement, consider the amount of pressure your expectations might put on the caregiver.
Telehealth provides increased opportunities for caregiver education and involvement. But, just like the transition from clinic to online can be challenging for clinicians, remember that caregivers might experience similar struggles.
Consider these questions when it comes to caregiver involvement:
- What is the role of the caregiver?
- Are they a family member? In-Home Supportive Services (IHSS)?
- How much caregiver education is required to ensure the patient’s safety?
- What is the caregiver’s level of supportive training?
- Does the caregiver feel comfortable in their role as e-helper? Is additional training required?
- If the caregiver is a family member, consider “caregiver burden” when adding additional roles (e.g. e-helper).
Best practices for actually delivering the telehealth assessment:
Telehealth delivery might still be novel, but your approach to delivering care likely won’t be. Here are some best practices to ensure your assessments run as smoothly online as they would in the clinic. You’ll probably see some familiar themes from when you first entered the clinical world. 🙂
Practice makes perfect prepared
There’s no such thing as perfect, but familiarizing yourself with your technology platform and materials will go a long way in making sure you have a smooth session. Don’t wait ‘til showtime to make a game plan. Practice in advance, and you’ll have a much easier time getting the results you want.
Turn to the experts
While telehealth is still brand-new to some of us, for others it’s not their first rodeo! You’ll definitely benefit from learning from those who have walked this path before you. Practitioners like Dr. Jana Cason have contributed a wealth of knowledge for telehealth best practices, including this tip-filled video that helps you cut down on planning time.
The Telehealth Resource Center also has a great etiquette checklist on some do’s and don’ts to help your sessions run smoothly. Some key tips include checking your lighting and eliminating unnecessary sound or visual distractions (this is not the time to take that fashion risk—think neutral colors!).
Assessment publishers like WPS (Western Psychological Services) and Pearson have offered guidance on how to use their products effectively. The APA (American Psychological Association) has also offered practical guidance on the administration of standardized assessments.
Phone a friend
If this is your first time administering an assessment via telehealth, consider phoning a friend or colleague to do a practice walkthrough. Chances are, your colleagues might be in the same boat and feel similarly grateful for the practice. Taking these steps to prepare yourself will help you to focus more fully on your client.
Set your clients up for success
You’ll want to prepare all session participants in advance. In addition to the client, this might mean a caregiver and/or e-helper. Help your client know what to expect in advance. Send an outline of the session goals (e.g. completing a certain assessment or teaching a home exercise program). Provide an estimated time to complete any assessments you choose. Make sure to include a supply list if you are not providing all of the materials needed. This is also a good time to request the session environment be cleared of unnecessary items and distractions. If this is your first online session with the client, send clear written instructions on how to access the video conferencing platform. Plan on the session taking a little longer to get them oriented, and make sure to budget that time accordingly so your assessment time will not be impacted.
Assessments for telehealth OT evaluations
Here is a list of assessments that have been used and/or studied by OTs in the telehealth setting.
BEERY-VMI – Neuro.
Found to be reliable when administered remotely. It is a non-verbal assessment that evaluates integration of visual and motor abilities. There are two forms: one for ages two through 18, and another for ages 19+. Guidance on administering the assessment remotely can be found on the publisher’s site.
Berg Balance Test – Balance.
A small feasibility study from 2007 looking at remote assessment of five widely used motor function measures found that ROM, MMT, items of the Berg Balance Test, and the TUG were all technically feasible to perform without significant differences from co-located measurements. They did address that while technically feasible, it may not always be feasible to safely administer certain measures.
Canadian Occupational Performance Measure (COPM) – ADLs and IADLs.
The electronic version is available for a small fee, and can be completed by the participant on their device. The COPM is client-centered and reveals the client’s self-perception of ADL and IADL performance over time.
Katz Index of Independence in Activities – ADLs and IADLs.
Screen for cognitive and physical impairments in older adults.
Lawton Instrumental Activities of Daily Living scale – Cognition.
Screen for cognitive and physical impairments in older adults.
Manual Ability Measure-16 (MAM) – Parkinson’s Disease (PD).
This assessment was found to have high interrater reliability in a study involving people with PD.
McMaster Handwriting Assessment Protocol (MHAP) – Pediatrics.
This test is available online. While it’s not norm-referenced, Melanie Criss, a school-based OTD, does recommend this assessment in this video.
Mini-Cog© – Cognition.
Screen for cognitive and physical impairments in older adults.
Mini Mental State Exam (MMSE) – Cognition.
Established to have good reliability (Martin-Khan, 2010; Kennedy, 2014; Herr, 2013). Evaluates short-term memory, visuospatial abilities, executive function, attention, language, and orientation to time and place.
Montreal Cognitive Assessment (MoCA) – Cognition.
Has been popularly examined and has been established to have good reliability (DeYoung, 2018; Lindauer, 2017) and good validity when administered via telehealth. Since September 2019, the MoCA can only be administered and scored by trained and certified individuals. Remote instructions for the administration (via telephone or videoconferencing) of the MoCA can be found by the publishers here. Evaluates short-term memory, visuospatial abilities, executive function, attention, language, and orientation to time and place.
Modified Barthel Index (MBI) – ADLs and Functional Mobility.
A Randomized Controlled Trial (RCT) just published in May 2020 in Southeast China found the Modified Barthel Index to be feasible, reliable, and valid when administered through a videoconferencing mobile app, compared to telephone administration.
Pediatric Evaluation of Disability Inventory – Computer Adaptive Test (PEDI-CAT) – Pediatrics.
Relatively quick to administer, computer-based, has a wealth of data to back its validity. Well-vetted norm-referenced questionnaire assessment of ADLs, participation, cognition, and motor skills.
Sensory Profile Measure and Sensory Profile 2 – Pediatrics.
The most commonly used valid and reliable questionnaire measure for children, according to a systematic review of sensory processing and modulation.
Short Form Everyday Technology Use Questionnaire (S-ETUQ) – Cognition.
Used in older adults to reliably assess an individual’s cognitive ability to utilize everyday technology. The questionnaire/interview focuses on the ability to use everyday technology, such as a remote control, household appliances, and a cell phone. Keep in mind that training is required to administer the ETUQ.
Timed Up and Go (TUG) Test – Functional mobility.
A small feasibility study from 2007 looking at remote assessment of five widely used motor function measures found that ROM, MMT, items of the Berg Balance Test, and the TUG were all technically feasible to perform without significant differences from co-located measurements. They did address that while technically feasible, it may not always be feasible to safely administer certain measures.
Visual Symptoms Assessment – Pediatrics.
Visual processing questionnaire that can be given to a caregiver to complete for their child.
WHO Disability Assessment Schedule II – Arthritis, SCI, CVA.
A culturally sensitive standardized measurement of 6 life domains, including functional mobility and ADLs.
Phone apps to make life easier
iPhone leveling app – This app was found to have good intra- and inter-rater reliability in a 2019 study published in AJOT.
iWalkAssess app – Free research-backed app to measure the 6-Meter and 10-Meter Walking Test, as well as the 6-Minute Walk Test, in post-stroke populations.
Conclusion
This article might feel a bit overwhelming, and that’s OK! Even when we’re not factoring telehealth into the equation, picking the right assessments for your patients can be a challenge.
But, as we lean into this new era of remote care, it’s exciting to see how assessments, both new and old, can be leveraged to give our patients our very best. This is an exciting time for the OT profession; we can now reach so many more patients without the barriers that once prevented them from seeking care! Here’s to a brave new world of care—and to our profession rising to the occasion to make it a wonderful place to be.
About the authors
Thank you to the OTD students, listed below, for their help with putting this article together! All of these authors are in their final term of OT school at Samuel Merritt University, with an anticipated graduation date of August, 2020.

Lisa Choromanski, OTDS – Lisa loves learning new things. Since graduating from San Francisco State University with a degree in art, Lisa has found herself exploring career opportunities in design, educational games, and holistic healing, to name a few. These passions have helped inform her view of occupational therapy. She is currently conducting a research project on the feasibility of using video game technology to increase upper-arm function in children with cerebral palsy. Apart from school, in no particular order, she loves hiking, eating cheese, listening to podcasts, and hanging out with her husband and three cats.

Tatiana Kreuzer, OTDS – Tatiana holds a BS from University of California, Davis with an emphasis on neurology, physiology, and behavior, along with a human development minor. Her 10+ years of experience working in children’s programming led her to pursue a career in occupational therapy. Observing and caring for children, and implementing strategies—while supporting and respecting their individual needs—has become a true passion of hers. She is currently conducting research to investigate the feasibility of a home-based protocol using FlintRehab’s MusicGloveⓇ device on children and adolescents with cerebral palsy. To this day, she aspires to be a pediatric OT, committed to providing children with the tools and skills they need in order to succeed. Outside of the OT profession, Tatiana enjoys spending quality time with friends and escaping to the beach.

Carolyn Shia, OTDS – Carolyn is interested in neurorehabilitation and working with individuals with neurological disorders. Prior to OT school, Carolyn worked as an accountant after graduating from Santa Clara University. She has since found her calling through occupational therapy and loves that the profession is guided by a holistic perspective. She is currently researching the provision of OT intervention via telehealth for the adult neurological population. Aside from studying OT, Carolyn enjoys rock climbing, doing yoga, taking walks, and papercrafting.

Jamie Stroppini, OTDS – Jamie is currently fulfilling her capstone project on the remote delivery of rehabilitation-based technology in children with unilateral cerebral palsy. Before OT school, she graduated with a degree in kinesiology. Jamie has 10+ years of experience in education, ranging from early intervention to transitional programs for young adults. Her creative mind and passion for empowering others to achieve their aspirations led her to a career as an OT—with the specific aim of facilitating technology within OT practice. Aside from OT student life, she enjoys DIY projects, attending sporting events, and discovering new movies/shows.
Thank you to Jana Cason, DHSc, OTR/L, FAOTA for taking the time to talk to our student authors during the writing process!

4 replies on “A Guide to OT Telehealth Assessments”
Wow! this is amazing. Thank you so much for sharing this amazing and useful information with us, you have got an interesting way of communicating the message in your blogs, really liked it,https://www.writomatic.co.uk/ keep bogging and keep sharing the useful work.
Can I simply just say what a comfort to find somebody that really knows what they’re discussing on the internet You definitely understand how to bring an issue to light and make it important. More and more people really need to read this and understand this side of your story.<a href=" https://www.writomatic.co.uk/"> Essay Editor </a> It’s surprising you’re not more popular since you certainly possess the gift.
Thank you for this interesting information! I am currently an OT doctoral student working on my project that entails looking at the use of telehealth in completing a home environment assessment and functional evaluation. Have you come across any assessments that have been used and proven to be beneficial for this avenue and area of practice?
Really helpful – thank you