Occupational therapy (OT) leverages the everyday experiences of individuals and communities to empower them in improving their health, well-being, and participation.
There are many ways for OT to occur in the community. Occupational therapy practitioners (OTPs) work in private homes, schools, community centers, shelters, and community-based clinics.
In this guide, we will focus specifically on “community-level” occupational therapy—that is, OT practice designed for large groups, communities, or populations. Our profession’s origins are actually rooted in this type of practice, with OT emerging alongside social reformers and movements like Jane Addams and the Hull House.

Community-level occupational therapy directs our skills as OT practitioners toward achieving sustainable, systems-level change that leads to broad and lasting impacts on health and well-being. These impacts often expand beyond individual outcomes to foster communities and systems that broadly support participation and health in the long-term.
You may have found this article because you ran into a community OT practitioner and want to learn more about their approach—or maybe you are wondering how you can involve occupational therapists in your own community-based work. Either way, we will do our best to cover the most important bases of community OT practice.
What Is Community Occupational Therapy?
At the community level, OT extends beyond individual interventions to address the occupation, health, well-being, and participation of entire groups, communities, or populations.
To do this, community OTs often design and launch programs to:
- increase access to daily meaningful activities, or
- facilitate meaningful activities that promote positive change.
These approaches are also used with individual OT intervention, but community OT programs scale them beyond a single individual or family. Community OT practitioners identify needs that exist across communities—and then develop programs and implement interventions that enhance collective well-being.
While community practice may take place in common clinical settings, it also includes:
- Client Engagement and Cohesion: Collaborating with multiple community members or organizations to identify goals and co-create solutions. This often means supporting community members in working better together.
- Activity Analysis: Examining and evaluating the everyday practices and routines of a community or organization. This can involve mapping processes or evaluating the community norms of everyday life.
- Promotion of Health: Designing initiatives that prevent injury and illness while promoting wellbeing, participation, and collective care. Health outcomes are often measured at the community or collective level.
- Adaptation and Technology: Modifying community spaces and systems to improve accessibility and participation for all members. This can involve changing the built environment, practices, or norms as well as incorporating assistive technology use into everyday community life.
- Policy Advocacy: Influencing policies to support inclusive and health-promoting everyday life in communities.This can involve supporting community advocacy efforts or providing expert consultation directly to policymakers.
As you can see, many of the same skills OT is known for in clinical or one-to-one settings are also used in community settings—but with a broader, expanded lens.
Thanks to Dr. Jenny Womack for her comment on LinkedIn encouraging us to display these approaches using a framework of the Socio-Ecological Model of Public Health. The figure below shows how these occupational therapy approaches might be understood across the layers of a society. While the layers of our communities aren’t so neatly compartmentalized, organizing various interventions this way reveals how different approaches might address varying aspects of the social and communal.
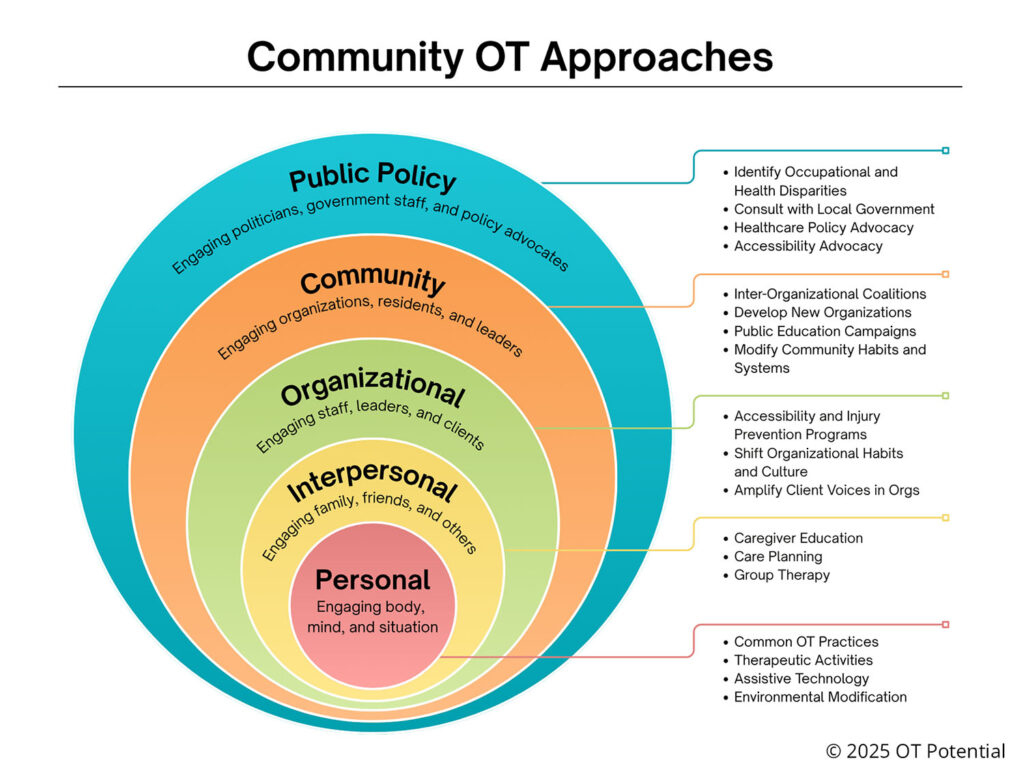
NOTE: In the Social-Ecological Model, “community” is a specific layer of society. In this post we use “community” more broadly to mean all of the layers beyond the individual.
Why is Community OT Needed?
Individual choices, diagnoses, or situations are not always the cause of poor health outcomes. Sometimes social norms, community systems, or routine ways of doing things in a society create differences in health among various groups of people.
Everyday life can present challenges or reinforce routines that create illness or affect health among community members. Community OT practitioners use the skills mentioned above to evaluate and intervene in those broader situations to improve community well-being. For example, community occupational therapy professionals might help with:
- Amplifying the voices of disabled community members.
- Advocating for more accessible transit systems.
- Consulting on the development of affordable housing for seniors.
- Addressing tensions among communities with changing populations and cultures.
- Fostering inclusion and awareness of dementia and cognitive differences.
- Coordinating home repairs and modifications for low-income families.
- And more!
When we address these issues at the community level, we can cultivate lasting change and sustainable healthy living within community systems. And when systemic or structural health disparities are identified, community-level OT is often the more appropriate and effective intervention to address those gaps broadly and long-term.
At the same time, we know that community-level changes and prevention efforts can reduce costs for both consumers and governmental programs such as Medicare and Medicaid. Building more accessible communities that encourage meaningful participation decreases the need for medical intervention and reduces the overall financial hardship experienced by individuals and communities alike.
Common Community OT Settings
Occupational therapy practitioners work in a variety of community settings, including:
- Community Centers: Offering programs for various age groups, from youth to seniors.
- Schools and Educational Programs: Leading programs and initiatives that provide school-based or community-wide support for students.
- Homeless Shelters and Transitional Housing: Developing programs that increase independent living skills. These programs may offer support to people living on the streets, disabled individuals seeking more independent housing, or women transitioning out of domestic violence situations.
- Workforce Development Programs: Supporting job readiness and vocational skills for individuals or training organizations and businesses to be more prepared to hire a diverse workforce.
- Public Health Initiatives: Participating in campaigns that promote disease prevention and wellness across communities, public spaces, or urban systems.
- Organizational Consultation: Providing guidance and technical assistance in implementing inclusive and strengths-based programs (for example, with museums or libraries).
These settings position OT professionals to address broader determinants of health and facilitate community-wide change. In the US, these settings are often situated outside of the healthcare system.
The Role of Occupational Therapy in Communities
In community settings, OTPs can play many roles—often in partnership with interdisciplinary teams that include social workers, public health professionals, urban planners, community organizers, human service professionals, and more. Similar to a clinical setting, there is some overlap among these professionals—but each brings their own contributions to the work. OTPs can be:
- Strategic Planners: Organizing community-wide efforts for vision development and goal-setting; creating action plans for achieving those goals.
- Program Developers: Designing and implementing initiatives that address identified community needs.
- Educators: Providing workshops and resources on topics like ergonomics, stress management, and healthy habits.
- Advocates: Influencing policies and practices that affect community outcomes.
- Collaborators: Partnering with other professionals, organizations, and community members to achieve shared goals.
- Consultants: Providing ongoing technical assistance and expertise related to initiatives, products, or programs in the community.
This collaborative and proactive approach is essential for fostering sustainable community development.
Is the OT Process Different in Community OT?
OTPs use the same process described in the Occupational Therapy Practice Framework (OTPF) for supporting change and health as they do in 1:1 therapy. However, the focus and scope of this process shifts.
Evaluation: Evaluation of community health, occupation, or everyday routines often involves gathering perspectives and data from multiple sources such as community leaders, organizations, targeted populations, census surveys, or other readily available community resources. Part of this stage is ensuring community members lead the way and drive the rest of the process. The final product can look like a Community Occupational Profile.
During this stage, OTPs may engage or leverage:
- Community advisory boards
- Community needs/capacity assessments
- Focus groups/town halls
- Already-available community data such as:
- AARP Livability Index
- Community oral histories
- Local census data
- Existing action plans
- Previous research studies
Intervention: Tailored and meaningful interventions at the community level are rooted in the community-level evaluation. Interventions broadly serve one or both of the following purposes:
- Increase access to participation in meaningful and healthy activities.
- Use everyday occupations and habits to support health and well-being.
Practitioners can suggest ways to modify community routines and practices, incorporate technology, or add new activities to benefit the community. Just as in 1:1 therapy, these need to be relevant to the context, routines, and culture of the community. Some frameworks for this work include:
- Community-based Practice
- Occupation-based Community Development
- Social Occupational Therapy
- Social Transformation through Occupation
Targeted Outcomes: The measurement of community-level outcomes should tie back to community interests and needs. While individual outcomes can be a part of this process (i.e., by aggregating many individual measures), it’s important to incorporate the measurement of cross-community perspective. Measurement options could include:
- Community health outcomes
- Program usage
- Completion of strategic plans
- Community satisfaction
- Changes in community culture or habits
Examples of Community-Level OT Interventions
Community-based OT interventions are diverse and tailored to specific populations and communities:
- Fall Prevention Programs: Educating seniors on home safety, facilitating access to home repairs and modifications, or providing balance exercise classes to reduce fall risk.
- Youth Engagement Initiatives: Organizing after-school programs that promote social skills and healthy routines or advocating for accessible places where youth can gather and build relationships.
- Mental Health Support Groups: Facilitating sessions that address coping strategies and community integration; organizing community activities that cultivate community care, mutual aid, and connection across differences.
- Accessible Transportation Projects: Collaborating on designs that accommodate individuals with mobility challenges; working with community members to advocate for local mobility options, particularly beyond driving.
- Coalition Building: Helping community members or organizations work better together and use coordinated tools for success; hosting gatherings of like-minded groups to brainstorm and problem-solve around specific community issues.
These interventions illustrate the adaptability and impact of OT within community contexts. OT interventions in the community typically involve analyzing systems through the lens of everyday life and identifying ways to improve outcomes.
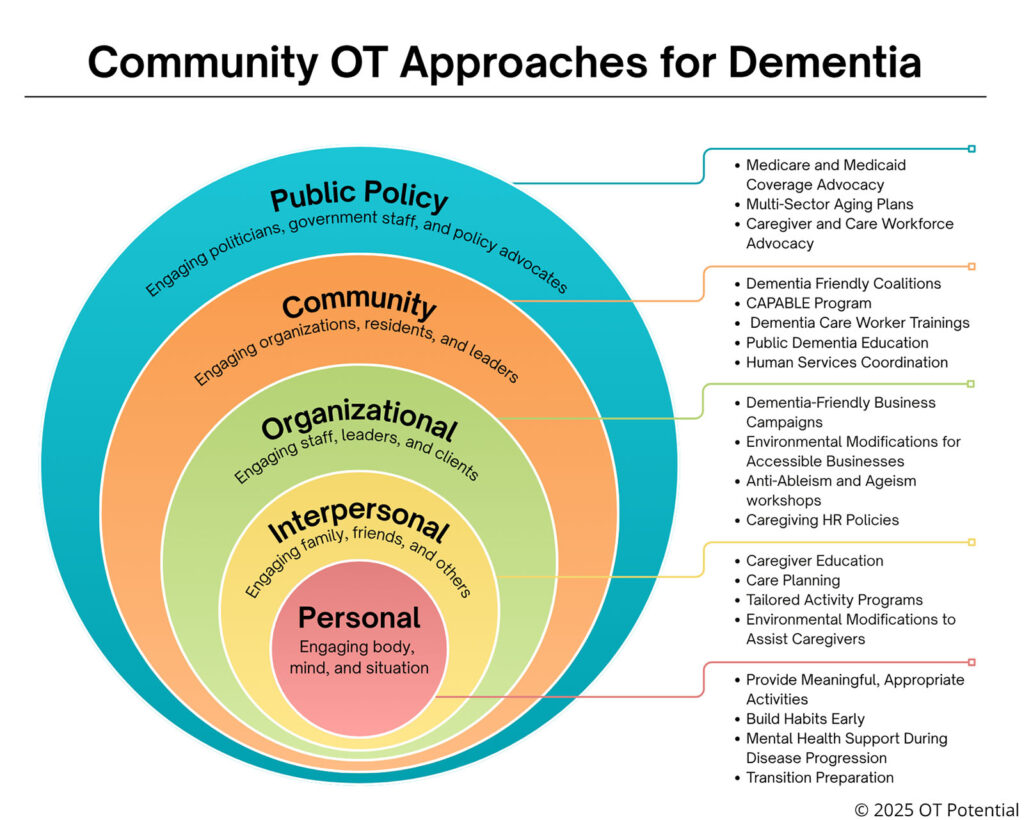
Below is an example of OT interventions focused on dementia and again organized with the Socio-ecological Model of Public Health. As you can see, an occupational lens and the skills of occupational therapy practitioners can be leveraged in many ways to address a single diagnosis or health concern across society.
Considerations for Working in Community OT
While community-level OT is greatly needed, practitioners should consider a few things as they embark on implementing this type of practice:
- Long-term Sustainability: Community work takes time, commitment, and trust with community members. The pace of progress is slower than 1:1 therapy, but the work is often dynamic and fast-paced—changing quickly in response to evolving community situations. Sustaining this relationship requires tempered approaches and strategies.
- Community Leadership: In 1:1 therapy, practitioners are assumed to have expertise, authority, and a certain ability to direct the approach of the therapeutic process. In community OT, community members must direct the work—and they may not readily see or appreciate the role or expertise an OT practitioner may bring. Practitioners must also let go of the authority position.
- Alternative Funding: In the US, occupational therapy is most commonly funded through healthcare mechanisms such as private health insurance, Medicaid, or Medicare. Funding for community practice often looks different given that the work is not tied to a specific individual or diagnosis. Grants, public health funds, private businesses or donors, and local government funds can all be sources for community OT work.
- Outcome Measurement: As with all OT practice, evaluating the impact of interventions is necessary; however measuring the impact of community work requires tools and measures tailored to community-level outcomes and goals.
Practitioners wanting to start or develop their involvement at the community level must make sure they have the skills and approach that address these aspects of the work.
How Does OT Complement Other Professions like Public Health and Social Work?
You might be wondering, “Isn’t this just public health interventions, social work, or even city and regional planning?”
Similar to how OTs work alongside physical, speech, and other therapists—as well as nurses and physicians—there are other disciplines that overlap in the community as they work to address broad challenges. Community OTPs often work in collaboration with social workers, public health professionals, city planners, and other community professionals.
Within this group, occupational therapy professionals are often the ones asking questions such as:
- What are things the community is already doing that can support this effort?
- How can we make this intervention accessible to more people?
- How might everyday community routines influence the way this plan unfolds?
- What are the concrete activities that are necessary to achieve this program’s goal?
- How can we modify expectations or ways of participation in these community activities to create more participation?
- What technology can we use to support greater engagement?
Find Community OT Professionals Near You
To find occupational therapy professionals who work in community settings, check out the OT Near Me Directory!
Resources for learning more:
- Community-based OT with Dr. Ryan Lavalley (Podcast Course)
- Occupational Therapy in Community and Population Health Practice (Book)
- The Occupation-Based Community Development Framework (Book Chapter)
- Social Occupational Therapy (Book)
- Social Transformation through Occupation (Case Study E-Book)
- International Social Transformation through Occupation Network (Networking Group)
- METUIA Social Occupational Therapy Laboratory (Research Lab)
- UNC Chapel Hill Community Practice Lab (Research & Program Development Lab)
Conclusion
Community-level occupational therapy is the tool through which occupational therapy practitioners can create widespread, systems-level change that leads to sustainable, healthier, and more equitable communities.
Community OT is a dynamic, evolving field that responds to the broad needs of many contexts. Leveraging the same tools that are so powerful in 1:1 therapy, community-based OTPs can build effective evidence-based programs that open more access to occupation, health, and well-being and promote occupation as a strategy for creating communities that are joyful, inclusive, and resilient.
If you have any feedback or questions about this page, please let us know in the comments!
