Here, you’ll learn all about pediatric occupational therapy. You can also find a pediatric OT near you!
Here’s what we’ll cover in this article:
- Find a pediatric OT near you
- What is pediatric occupational therapy (OT)?
- Would your child benefit from OT?
- Pediatric OT services by setting
- Starting OT early
- What does your first visit with a pediatric OT look like?
- Common pediatric OT interventions
- Evidence-based practice in pediatric OT
- How to become a pediatric OT
- Family resources
- Conclusion
Find a pediatric OT near you!
Pediatric OT professionals work in many different settings and have many different focus areas. Find the pediatric OTs near you on the OT Directory.
What is pediatric occupational therapy (OT)?
Occupational therapists (OTs) help people do the things they need (and want) to do in their daily lives. When a developmental delay, illness, or injury makes daily life difficult, OTs step in to help.
Pediatric OTs help kids with health struggles be, well, kids! That means guiding them toward becoming as independent as possible in things like play, self-care, feeding, dressing, and managing big feelings.
Your OT will work closely with your family, your healthcare team, and others who support your child on a daily basis. OTs are unique in their holistic approach to care, focusing on your child’s day-to-day activities.
Would your child benefit from OT?
Your child may benefit from OT if you would like extra support in helping them participate in the activities and routines that are common for other children their age. (This CDC guide to developmental milestones gives you an idea of the skills other kids are typically performing at various ages.)
You may work with an OT as early as in the NICU (i.e., when your child is an infant). You can also see OT professionals in an outpatient setting, through early intervention visits in your home, in a mental health setting, or as part of the school system. OTs can also support adolescents and young adults as they transition into the daily activities of adulthood.
OTs can support your child in many daily activities, including:
- Getting dressed
- Eating with the family and consuming a variety of foods
- Regulating emotions and using coping skills
- Advocating for themselves
- Handwriting and other school-related tasks
- Managing chronic pain
- Playing with friends safely
- Supporting their mental health and self-esteem
- Developing self-determination skills
- Grooming and hygiene skills, such as brushing their teeth
- Developing healthy sleep habits and routines
- Understanding their sensory processing experiences
- Organizing their personal areas (like their desk, backpack, and bedroom)
OTs support children with and without diagnosed conditions. Some common childhood conditions we are well-suited to address include:
- Anxiety
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- Autism Spectrum Disorder (ASD)
- Cerebral Palsy (CP)
- Conduct Disorder
- Chromosomal Disorders
- Depression
- Down Syndrome
- Dyslexia
- Emotional Disability
- Feeding Challenges
- Fetal Alcohol Spectrum Disorders
- Fragile X Syndrome
- Functional Neurological Disorder
- Hearing Loss
- Intellectual Disability
- Learning Disorders
- Muscular Dystrophy
- Oppositional Defiant Disorder (ODD)
- Obsessive-Compulsive Disorder (OCD)
- Pelvic Health Conditions
- Premature Birth
- Post-Traumatic Stress Disorder (PTSD)
- Postural Orthostatic Tachycardia Syndrome (POTS)
- Sensory Processing Disorder
- Spina Bifida
- Tourrette Syndrome
- Traumatic Brain Injury
- Vision Loss
Pediatric OT services by setting
Pediatric OT in hospitals
- What this setting offers: Children may receive OT services as an inpatient in the hospital while recovering from an acute injury or illness. Typically these services are part of a multidisciplinary rehabilitation care plan to address a child’s short-term needs for recovery so they can return home.
- Getting started: Inpatient therapy services are coordinated by your child’s doctor, nurse practitioner, or other prescribing provider. You may also be referred to outpatient therapy services upon discharge to continue to support your family while your child returns to their regular routines at home.
- Cost and funding: Health insurance policies often help cover the cost of medically necessary pediatric therapy services. Check with your hospital to see if financial counselors are available to assist with financial estimates and answer questions about coverage. Your insurance provider can also offer estimates for any out-of-pocket amounts you’ll need to pay.
Outpatient OT clinics
- What this setting offers: Outpatient occupational therapy helps children and teens develop the physical, cognitive, sensory, and social-emotional skills they need to function in daily life. The timing and duration of therapy depends on your family and your child’s needs, but often this looks like weekly 1-hour sessions, with goals reevaluated every few months. Because play is such a crucial occupation for children, outpatient therapy is often play-based and fun—kids might not even realize they are learning and developing important life skills!
- Getting started: Whether you need a physician’s order to start OT services depends on both your health insurance policy and your state’s regulations. Most states require physician orders for occupational therapy treatment, though many also have some form of direct access enabling clients to see an OT without a referral. Even with direct access, however, insurance policies often require a referral for coverage. Your child’s pediatrician can make a referral for outpatient OT based on your family’s needs and location.
- Cost and funding: Health insurance may help cover the cost of pediatric therapy services. Your clinic’s billing team or your insurance provider can assist with cost estimates and payment options.
Early intervention OT
- What this setting offers: Early intervention therapists work with families of young children (usually from birth to age 3) who have developmental delays or disabilities that impact their everyday activities. Therapy sessions usually take place at home, and caregivers are highly involved. Early intervention OTs can teach caregivers techniques for supporting their child’s development and making everyday tasks easier.
- Getting started: Infants and toddlers first receive an evaluation to determine if they are eligible for the state’s early intervention program. If eligible, the program team works to develop an Individualized Family Service Plan (IFSP), which outlines treatment goals and the services your family will receive. To request an evaluation, talk to your pediatrician or local Early Intervention Program.
- Cost and funding: Early intervention services are often funded by government programs like Medicaid or state early intervention programs, so they may be free or low-cost to families. Sometimes private insurance plans also cover these services. It’s a good idea to check with your insurance provider and your local early intervention program to understand the costs and available funding.
OT in schools
- What this setting offers: School-based OTs help kids participate in their schooling by conducting evaluations, teaching specific skills, recommending environmental changes, and providing education and resources to teachers. This guide and directory provide answers to basic questions about school-based occupational therapy.
- Getting started: As part of Child Find, teachers and parents can request an evaluation for OT services for a student if a disability or delay is suspected. If you have a concern, you can get the ball rolling by talking with your child’s teacher and school district to request an evaluation.
- Cost and funding: Most public schools use federal, state, and district funds to provide therapy services to students who qualify—at no cost to families, regardless of insurance status.
Mental health settings
- What this setting offers: OTs in mental health settings—sometimes called psychiatric or behavioral health settings—help children and adolescents develop skills and strategies to manage their emotions and improve their well-being. Occupational therapists work in both inpatient and outpatient mental health settings, often delivering mental health care via group therapy.
- Getting started: If you have a concern about your child’s mental or behavioral health, discussing it with your pediatrician is a good first step. They can refer your child to an OT for an evaluation—or initiate admission to a behavioral health hospital, if necessary.
- Cost and funding: Insurance policies may include coverage for behavioral health care, including occupational therapy. Check with your insurance provider and/or treatment facility to understand your estimated costs and options for payment.
Seek occupational therapy early!
Typically, the sooner we start working with your child, the better the outcomes. If you have any concerns about a delay in your child’s development, don’t hesitate to seek out an OT.
In the United States, early intervention is required by a federal mandate (known as IDEA) specifying that schools must find and evaluate students who may have disabilities—at no cost to families. This covers children from birth to 21.
You can read about IDEA here. Child Find is a resource that walks you through reaching out to your school if you have a concern about a delay. This program may not cover all of your OT needs, but it is certainly a good place to start!
Here are other ways to start your OT journey:
- Discuss OT with your child’s pediatrician
- Call your school district
- Seek early intervention services in your community
- Talk with your teacher
- Look up local occupational therapy clinics and give them a call for more information
- Use the OT Potential Directory! (See our pediatric OTs above.)
What does your first visit with a pediatric OT look like?
During your first visit, an OT will evaluate your child. Their goal is to get to know your child and your family to determine if OT treatment is a good fit for you.
The OT will ask questions about your concerns, your goals, and what a typical day looks like for your child and family. Your child will be included in the evaluation as much as possible—their voice is important, and therapy is most effective when they play an active role in planning.
The OT will usually want to observe your child doing some everyday tasks, too. There might also be formal assessments, based on your situation.
Common pediatric OT interventions
OTs are focused on delivering pediatric interventions that make a real, lasting difference in your child’s life. We use multiple approaches to accomplish this, including:
Educating parents and caregivers
If your child has a new diagnosis, part of the journey for your family is learning how it impacts your lives. As OTs, we typically spend more time with kids and their families than other medical providers do. We take our role in helping you learn about, and cope with, a new diagnosis very seriously. Our main objective is making your daily life as easy as possible.
Improving physical/emotional/cognitive skills
Sometimes, difficulty with a specific skill can make your child’s day extra tough. We can often help them improve that specific skill through targeted training or learning. An example would be strengthening the muscles in your child’s arm or hand in order to improve their ability to feed themselves or get dressed. Another example would be teaching them a new way of responding to tough social situations.
Providing a safe and supportive place to try new skills
OTs often work with children who have complex health conditions. Part of helping them learn to navigate their day is providing a safe space for them to trial-and-error new skills. OTs want to find solutions that work for your and your family. So, we teach children to use their strengths and learn what works for them. In our work, there are rarely cookie-cutter answers. Everything is tailored to you and your child.
Recommending technology and environmental changes to support your child
When we reach the limits of improving certain skills, we can often use technology or recommend changes to your child’s environment to get them the rest of the way. For example, your child may benefit from a wheelchair and some tweaks to your home to make it more wheelchair accessible.
Or, maybe your child is having difficulty sleeping. Changing the lighting and noise levels in their room—or using a sound machine—can help a lot.
Teaching self-advocacy
Our goal is to teach your child skills they can use long after therapy has ended. We want them to learn about their challenges, embrace their diagnosis, understand their strengths, and feel confident asking for what they need.
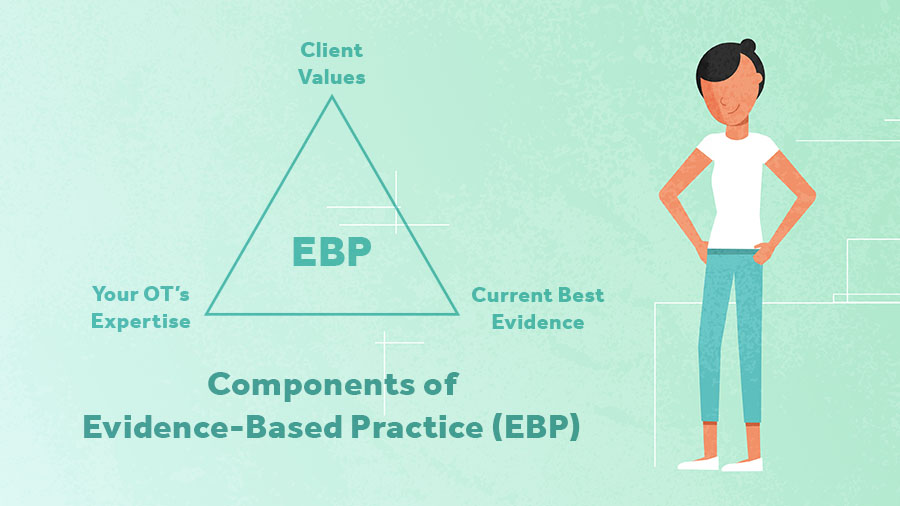
Evidence-based practice in pediatric OT
Occupational therapists are proud to use evidence-informed practice. That means we base our treatments on science and research. But, that does not mean there are cut-and-dried solutions for everything. Every child’s goals, intervention approaches, and therapy sessions are different, because every child is different.
To us, evidence-based practice means we are always balancing three things:
- What is important to you and your child
- Our own experience and expertise
- The latest research
To see an example how we digest the evidence behind our interventions, please see our pediatric interventions blog post.
How to become a pediatric occupational therapist
Occupational therapists work with people across the lifespan to make daily life easier and more enjoyable. Those who work with children are passionate about uncovering each child’s strengths and capabilities to help families thrive. So, what does it take to become a pediatric OT?
Occupational therapists (with titles such as OT, OTR, ORL/L, MSOT, OTD) must hold a master’s degree or a clinical doctorate in occupational therapy. They also must be certified by the National Board of Certification in Occupational Therapy (NBCOT). (Note that OT professionals who entered the field prior to 2007 might practice with a bachelor’s degree.) Additionally, OTs must be licensed to practice in their specific state.
Occupational therapy assistants (OTA, COTA), who collaborate with OTRs to provide therapy services, must earn an associate’s degree in occupational therapy. COTAs also receive certification from NBCOT and must be licensed to provide services in their state.
Pediatric occupational therapists do not need to specialize in pediatrics to work with kids, but there are tons of certifications and trainings to help practitioners hone their skills and gain knowledge in specialized domains. Some common pediatric-related specializations you might come across include:
- Assistive Technology Professional (ATP)
- Seating and Mobility Specialist (ATP/SMS)
- Basic DIRFloortime Certification
- AOTA Board Certification in Pediatrics (BCP)
- Certified Autism Specialist (CAS)
- Certified Psychiatric Rehabilitation Practitioner (CPRP)
- Certified Hippotherapy Clinical Specialist (HPSC)
Family Resources
For parents who want to learn more about their child’s diagnosis or find more resources to help them support their child at home, we’ve complied a list of books that are commonly recommended by pediatric OTs. If you have found a helpful resource that isn’t on this list, let us know in the comments so we can share it with more families!
- ADHD is Our Superpower (ADHD)
- Connections Over Compliance
- The Explosive Child
- The “How to Talk” Series
- The Out-of-Sync Child (Sensory Processing)
- The Out-of-Sync Child Has Fun (Sensory Processing)
- The Power of Showing Up
- Trauma-Responsive Pedagogy
- Uniquely Human (Autism)
- The Whole-Brain Child
Conclusion
It can be hard to see your child struggling. We want you to know that OTs are here to support you and your child. Each and every kid out there possesses unique and wonderful strengths. Having support from a concerned adult—like you, dear reader—can make a huge difference in their ability to thrive.
We look forward to working with you and your child. Our goal is to leverage both your child’s strengths and your support to make daily life easier for your whole family.
Posts for related pediatric OT questions
How do I become a pediatric OT?
What certifications can pediatric OTs obtain?
How much does an OT make?
Where can I find pediatric OT continuing education courses?
Where can I find a pediatric OT job?
How do I write a pediatric SOAP note?
Where can I find influential pediatric OT research?






