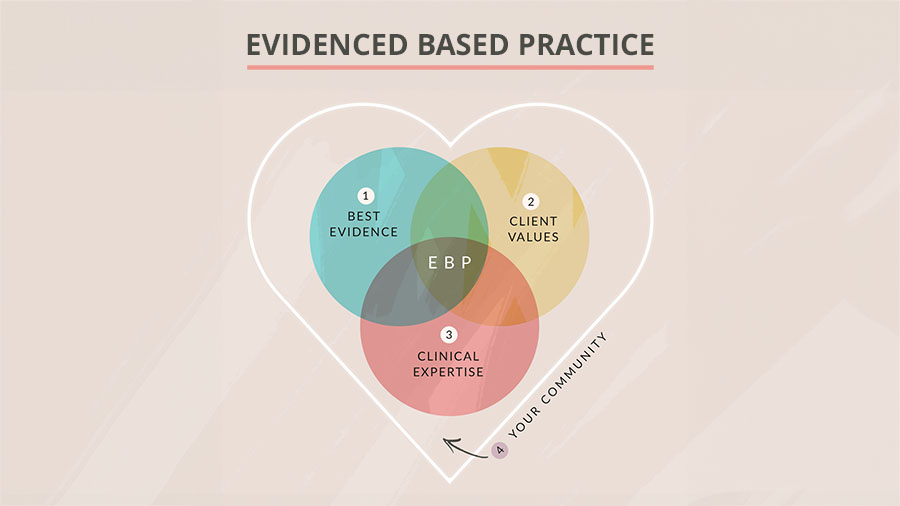
Occupational therapy practitioners turn to evidence-based practice (EBP) for many reasons.
We look for answers, treatment recommendations, and affirmation that we’re truly providing the best possible care to our clients.
But while EBP is considered the gold standard for improving healthcare practices, there is still a lot of debate on how it should be defined and applied.
In this article, we explore the purpose of evidence-based practice in occupational therapy and offer practical strategies for building a strong, well-rounded evidence base to support your OT practice.
This article covers:
Preamble: Why EBP Matters in OT
1. Best Evidence
2. Client Values
3. Clinical Expertise
4. Your Community
Why Evidence-Based Practice Matters in OT
Let’s take a step back and start with an actual definition of evidence-based practice.
According to this paper, evidence-based practice is “the conscientious, explicit and judicious use of the best evidence in making decisions about the care of the individual patient.”
Essentially, EBP takes the assessments and interventions supported by the latest research and incorporates them into care in a way that aligns with patient needs.
While evidence-based practice is still considered the gold standard for high-quality healthcare, there has been a push over the last few decades to move toward evidence-informed practice, in which practitioners seek to become “knowledgeable about findings coming from all types of studies and to use them in an integrative manner, taking into consideration clinical experience and judgment, clients’ preferences and values, and context of the interventions.” Evidence-informed practice, therefore, is broader and more inclusive of various forms of knowledge.
While the term “evidence-based” is used throughout this article for consistency and clarity, you may notice that the model of EBP presented here is actually more reflective of evidence-informed practice.
Now let’s talk about WHY we really care about the evidence.
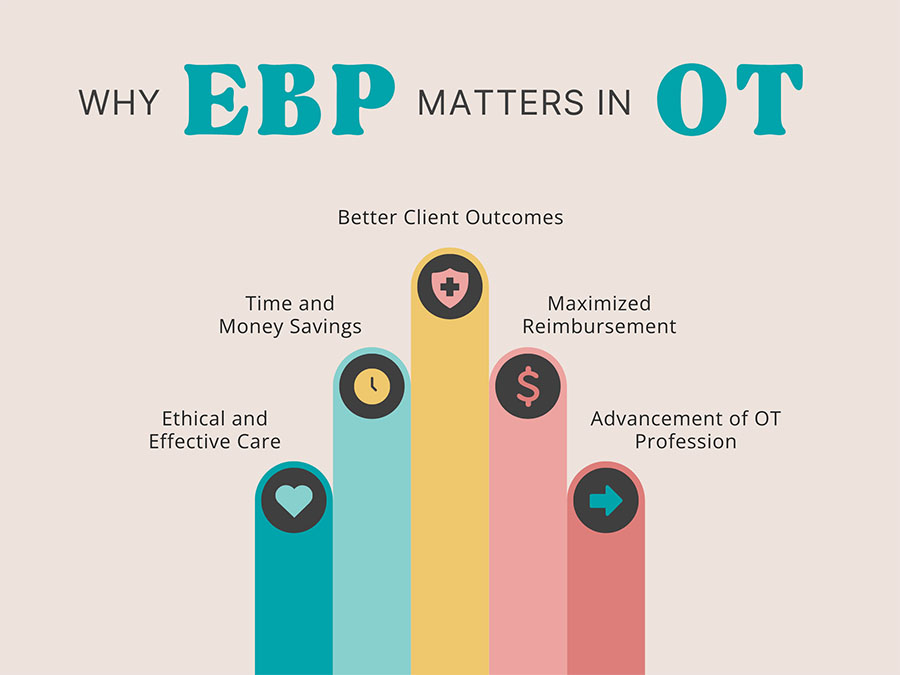
Considering how busy we are in our day-to-day practice as OT practitioners, it’s worth looking critically at why EBP matters to us.
It turns out that EBP produces better outcomes in a more cost effective way compared to non-evidence-based treatment approaches. By moving toward EBP, we’re likely streamlining our busy schedules—and ultimately, giving our patients better care (and hopefully saving them time and money in the process)!
Healthcare professionals—including OTs and OTAs—should use EBP to identify practices to eliminate just as much as they use it as a guide for practices to add.
The primary goal of EBP is utilizing research evidence to decrease the use of ineffective healthcare practices and support the delivery of ethical, effective, and optimal treatment.
In other words, EBP helps you ditch the ineffective treatments and replace them with those proven to work.
While this sounds obvious, it is actually much harder to change your professional habits than you may think. If you want to do some extra reading on this, I highly recommend the article, ”When Evidence Says No, But Doctors Say Yes.”
EBP is also:
- A highly valued ideal of the American Occupational Therapy Association (and a pillar for the AOTA Vision 2025).
- Essential from a reimbursement perspective, as payers use it as a framework for evaluating the necessity of interventions. In fact, EBP serves as a guide for reimbursement of services—especially with Medicare’s increased emphasis on value-based payment initiatives.
EBP requires that occupational therapy practitioners collaborate with their patients, use valid and reliable information, and balance openness to new ideas with rigorous clinical scrutiny.
Expert occupational therapy professionals hone their expertise by constantly questioning and learning from their clients, the evidence, and the overall context of their lives. So, what does that look like?
1. Best Evidence
Let’s talk about research evidence. As OT practitioners, we want to use the best available information to guide our clinical decision-making. But on top of seeing clients, completing required documentation, and meeting productivity standards, most of us just don’t have the time to find and absorb every single study relevant to our practice area.
Practice guidelines provide a shortcut to identifying EBP recommendations. Grounded in a thorough analysis of current research literature, these recommendations are typically graded based on the strength of the supporting evidence. This makes it easy for clinicians to decide which practices are worth trying and keeping—and which ones we should ditch.
The process of developing high-quality clinical practice guidelines is rigorous. If you are curious about these methods, check out the GRADE framework for evaluating guideline quality.
Reviewing recent and reputable practice guidelines is a great way to quickly gain a big-picture understanding of the current evidence on a particular condition or patient population, but the guidelines can’t answer every clinical question—nor should they!
Guidelines are meant to inform practice, not direct it. When reading guidelines, you will often get a sense of where your OT treatment fits into a comprehensive care plan. Guidelines also help you confirm that you are covering the most essential aspects of care for a particular diagnosis. At times, you can also use the free clinical practice guidelines and systematic reviews below to better understand the risks and benefits of different OT treatment options.
Free Clinical Practice Guidelines
But, what exactly does this best evidence actually look like?
To give you concrete examples, we are providing links to open access practice guidelines and systematic reviews that have been published in the past 5 years and provide guidance relevant to occupational therapy. Not all practice guidelines are equally valid or reflect the best and most current evidence. Please use your own discretion when applying guidelines.
This of course, is meant to be a starting point, in your quest to find the right research. You will be able to find even more guidance on accessing evidence in our upcoming post on knowledge translation.
Here’s the categories of guidelines you are going to find below:
- AOTA Guidelines
- KITE UHN Guidelines
- RCOT Guidelines
- WHO Guidelines
- Reviews with OT Potential Courses
- Neurological Conditions Reviews
- Pediatrics Reviews
- Additional Systematic Reviews
- Resources for Finding Clinical Practice Guidelines




Systematic Reviews with Implications for Occupational Therapy
Reviews with OT Potential Courses
Constraint‐Induced Movement Therapy In Children With Unilateral Cerebral Palsy
Cochrane Database of Systematic Reviews, 2019
🎧 OT Potential COURSE
Depression In Neurodegenerative Diseases
Neuroscience & Biobehavioral Reviews, 2019
🎧 OT Potential COURSE
Diagnosis and Treatment of Parkinson Disease
Journal of the American Medical Association, 2020
🎧 OT Potential COURSE
Effectiveness of OT for Children With Disabilities
Australian Occupational Therapy Journal, 2019
🎧 OT Potential COURSE
Non-pharmacological interventions for Spasticity In Adults
Annals of Physical and Rehabilitation Medicine, 2019
🎧 OT Potential COURSE
Psoriatic Arthritis Guideline
Australian Occupational Therapy Journal, 2019
🎧 OT Potential COURSE
Preventing and Treating Children With Cerebral Palsy
Current Neurology and Neuroscience Reports, 2020
🎧 OT Potential COURSE
Neurological Conditions
Canadian Guideline For Parkinson Disease
Canadian Medical Association Journal, 2019
Guidelines On The Progressive Ataxias
Orphanet Journal of Rare Diseases, 2021
OT Recommendations for Functional Neurological Disorder
The Journal of Neurology, Neurosurgery, and Psychiatry, 2020
OT For Cognitive Impairment In Stroke Patients
Cochrane Database of Systematic Reviews, 2022
Pediatric Mild Traumatic Brain Injury
Annals of Emergency Medicine, 2023
Rehabilitation for People with Multiple Sclerosis
Cochrane Database of Systematic Reviews, 2019
Telerehabilitation services for Stroke
Cochrane Database of Systematic Reviews, 2020
Time Spent In Rehabilitation On Activity Limitation And Impairment After Stroke
Cochrane Database of Systematic Reviews, 2021
Pediatrics
Cerebral Palsy In Children: A Clinical Overview
Translational Pediatrics, 2020
Guideline For The Treatment Of Juvenile Idiopathic Arthritis
Arthritis and Rheumatology, 2022
Interventions To Improve Physical Function For Children And Young People With Cerebral Palsy
Developmental Medicine and Child Neurology, 2022
Pediatric Teleheath
Physical and Occupational Therapy in Pediatrics, 2021
Rehabilitation Among Children With Cancer
CA: A Cancer Journal for Clinicians, 2023
Rehabilitation of Chronic Pain: Pediatric Pain
Journal of Clinical Medicine, 2019
Additional Systematic Reviews
Complex Regional Pain Syndrome Guidelines
Pain Medicine, 2022
Exercise, Rehabilitation, Diet, And Additional Integrative Interventions For Rheumatoid Arthritis
Guideline Central, 2023
Obesity In Adults: A Clinical Practice Guideline
Canadian Medical Association Journal, 2020
Occupational Therapy Interventions In Chronic Pain
Occupational Therapy International, 2015
Occupational Therapy For Epidermolysis Bullosa: Clinical Practice Guidelines
Orphanet Journal of Rare Diseases, 2019
OT For Mental Health Conditions And Substance Use Disorders
Canada’s Drug and Health Technology Agency, 2023
Reducing Physical Activity Limitation And Preventing Falls In Older People With Visual Impairment
Cochrane Database of Systematic Reviews, 2019
More helpful resources for finding clinical practice guidelines
In compling the above list, here are the resources we found most helpful.
- American Occupational Therapy Association (AOTA)
- Cochrane Library
- ECRI Guidelines Trust
- European Alliance of Associations for Rheumatology (EULAR)
- Evidence-Based Review of Stroke Rehabilitation (EBRSR)
- GIN International Guidelines Library
- Guideline Central
- KITE UHN
- TRIP Medical Library
Do you know of a great free practice guideline missing from this list? Let us know in the comments!
Don’t see a guideline for your client population? Many emerging areas of practice lack enough literature to develop rigorous practice guidelines, but more are being developed all the time. The TRIP database reveals ongoing systematic reviews in areas such as the effectiveness of equine assisted OT, support for leisure and sexuality occupations, and school-based OT!
2. Client Values
Asking the Right Questions
Ultimately, occupational therapy should be designed around the client’s needs, preferences, and individual context. Open-ended questions and reflective listening go a long way toward opening up communication with clients and creating a collaborative environment. This spirit of curiosity can also strengthen your practice by ensuring your assessments and interventions are truly in line with what matters most to your clients and their families.
To do this, we can use the O.A.R.S. strategy from the therapy technique Motivational Interviewing (MI)—which aims to strengthen the motivation for change by using evocative questions to build a collaborative and empathetic relationship.
O.A.R.S. is a handy acronym for:
Open Ended Questions: Invite more detailed responses than yes/no questions.
Affirmations: Recognize the client’s values, efforts, and preferences.
Reflections: Validate and acknowledge what the client is saying.
Summaries: Clarify what was said.
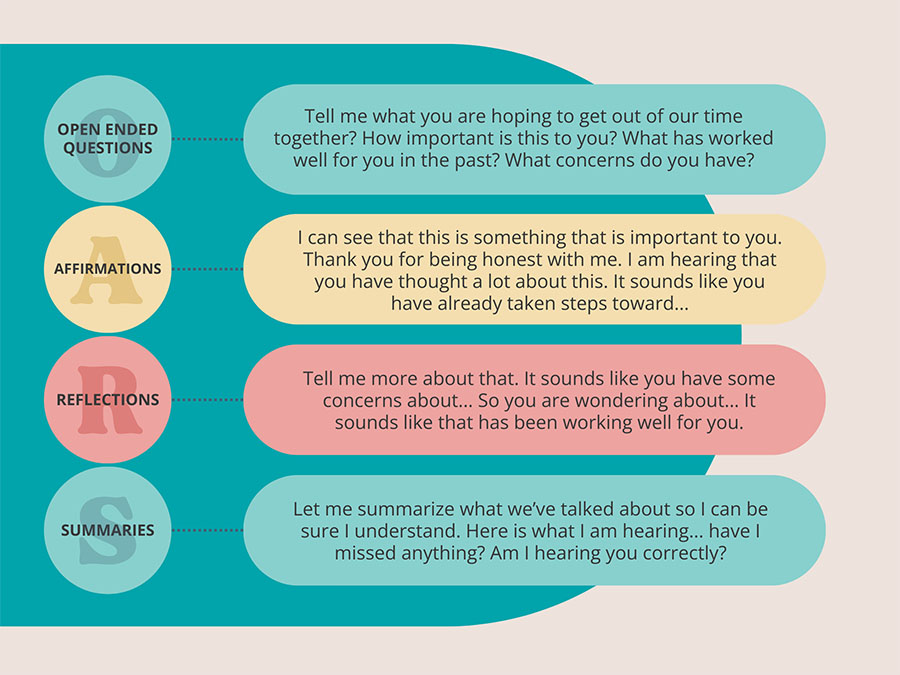
Words are powerful! Small changes in phrasing can make a big impact on how clients feel about and engage with therapy. Remind yourself of this handy acronym the next time you step into a client evaluation or treatment session.
For even more helpful MI tips, check out “3 Motivational Interviewing Strategies for OTs.”
Using Client-Centered Assessments
Assessments lay the groundwork for building effective OT interventions for each client. Client-centered assessments—like self-report measures or semi-structured interviews—offer a helpful way to establish your client as a partner in care.
Learn more about choosing the right occupational therapy assessments here. If you’re a member of the OT Potential Club, you also have access to our comprehensive OT Assessment Search.
3. Clinical Expertise
Your clinical expertise is a culmination of all of your professional experience and education.
But, how do clinicians take this massive amount of insight and make it actionable?
One cognitive short-cut we’ve found many therapists express is the development of what we call “personal paradigms.” These ways of thinking help us consider how new information fits in with our own beliefs, assumptions, philosophies, existing knowledge, schedules, capacities, and environments—all at once!
This is why different occupational therapy practitioners presented with the same client and same evidence might still take very different approaches to assessment and intervention. The process of filtering information through our personal paradigms is complex and deeply personal, and it often happens subconsciously.
If you have time, check out this editorial about “mindlines,” the internal guidelines we each develop over our lifetime.
There are no straightforward or simple tools for honing this aspect of evidence-based practice, because this part is YOU.
That being said, one strategy that can help us be more reflexive and self-critical about our clinical decision-making is simply identifying our personal paradigms. Bringing awareness to these often-subconscious considerations can save us from falling into the trap of becoming complacent in our routines by challenging us to question how our knowledge, beliefs, and behaviors align.
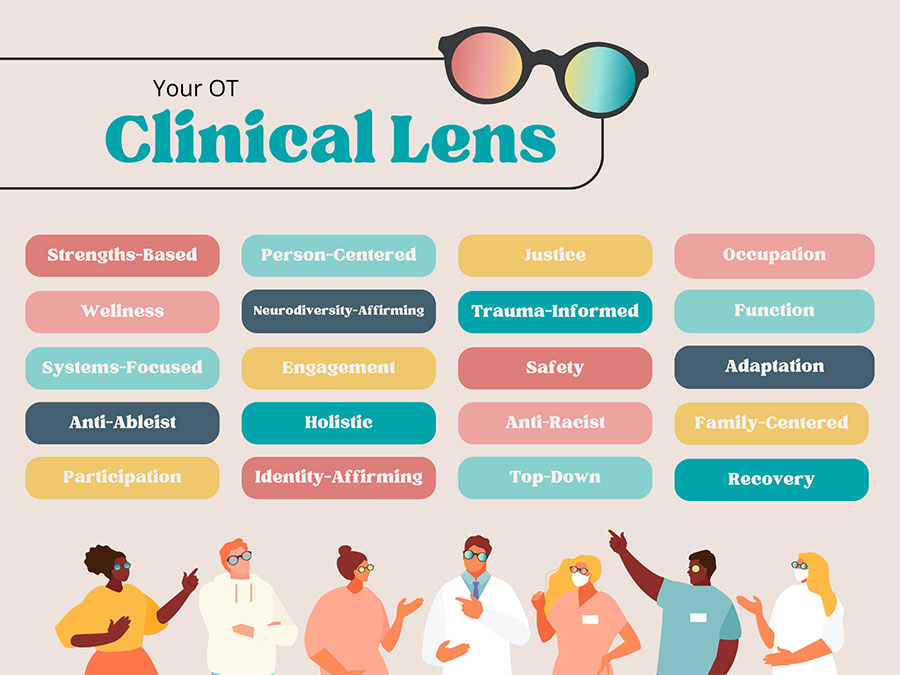
Take a moment to identify the paradigms that are most apparent in your practice. Do you consider yourself a neurodiversity-affirming provider? Is trauma-informed care at the center of what you do? Do you value top-down approaches or strengths-based practices? Each of these perspectives color your clinical lens and shape what EBP looks like for you.
Your clinical lens directly impacts the way you filter and apply evidence. Evidence, in turn, shapes how your clinical lens evolves and changes over time as you internalize new knowledge and shed the practices and mindsets that don’t serve your clients.
4. Your Community 💜
Our fourth dimension of evidence-based practice is your community, the context in which EBP truly takes form. This dimension is not found in traditional EBP models, but I believe is crucial to consider explicitly because of its massive impact. No OT is an island! As occupational therapy professionals, we learn just as much (if not more) from our mentors, colleagues, and experts in the field as we do from research studies and practice guidelines.
While some proponents of EBP might see this informal exchange of knowledge as a barrier to the adoption of formal research evidence, I believe it is necessary to lean on our communities in order to contextualize knowledge in real-world settings and fill in the wide gaps that research evidence doesn’t address.
In addition to your IRL community, you can connect with a global community of occupational therapy professionals and students—and even clients!—when you sign up for the OT Potential OT Directory. And, you’ll find even more groups to join in our post on OT forums and communities.
Conclusion
The art and science of occupational therapy is built upon an expansive and diverse knowledge base. Providing the best possible care to our clients requires a careful balance of the best evidence, our clinical expertise, and our clients’ values and preferences. I hope this article has helped you reflect on the nuances of EBP in OT practice and identify ways to strengthen your own evidence base.
Resources
Baker, N., & Tickle-Degnen, L. (2023). Evidence-based practice: integrating evidence to inform practice. In B. A. B. Schell, G. Gillen, & M. E. Scaffa (Eds). Willard and Spackman’s Occupational Therapy (14th ed.). Philadelphia: Lippincott Williams & Wilkins.
Rosengren, D. B. (2018). Part II: Engaging. In Building Motivational Interviewing Skills: A Practitioner Workbook (2nd ed.). essay, Guilford Publications.
Taylor, R. R. (2023). Kielhofner’s research in Occupational therapy: Methods of inquiry for enhancing practice (3rd ed.). Philadelphia: F.A. Davis Company.
